Obesity is a long-term medical condition where excess body fat builds up to the point that it may have a negative effect on health.
The accumulation of an excessive amount of body fat can cause type 2 diabetes and the risk of type 2 diabetes increases linearly with an increase in body mass index.
Obesity is a complex, chronic condition influenced by genetics, behaviour, environment and social factors.
It’s typically measured using the Body Mass Index (BMI), which compares a person’s weight to their height.
A BMI of 30 or above is considered obese (or 27.5 for South Asians) while a BMI between 25 and 29.9 is classed as overweight.
However, BMI doesn’t always tell the full story — where fat is stored in the body, especially around the abdomen, can play a big role in disease risk.
How does obesity develop?
Obesity develops over time when a person consistently consumes more calories than their body uses.
These excess calories are stored as fat. Although this sounds simple, the causes of obesity are anything but. It’s not just a matter of willpower — a range of physical, emotional, environmental and social factors come into play.
Modern life makes it easy to gain weight. Many people work in sedentary jobs, spend hours in front of screens and rely on convenience foods that are high in calories but low in nutrients.
Stress, poor sleep and certain medications can also lead to weight gain.
People living in deprived areas may find it harder to access healthy food or safe places to exercise.
Genetics can influence how your body stores fat, how hungry you feel and how your metabolism works. The result is that millions of people struggle with obesity, even when they’re trying to live a healthy life.
Obesity in the UK
The UK has the highest level of adult obesity in Western Europe.
According to the latest Health Survey for England, around 26% of adults are classified as obese and an additional 38% are overweight.
That means nearly two-thirds of adults in the UK are carrying excess weight.
The numbers are equally concerning for children, with nearly one in three children aged 10 to 11 now classed as overweight or obese.
Forecasts suggest that by 2040, more than 70% of UK adults could be overweight or obese if action isn’t taken. Obesity is now one of the leading causes of preventable ill health and early death in the UK — and it’s also placing enormous strain on the NHS.
- Preadolescent obesity risk in offspring reduced by breastfeeding
- Research shows weight loss doubles with early use of anti-obesity medication
- New fat cell subtypes could transform obesity care
Symptoms and signs of obesity
Obesity doesn’t always present immediate symptoms, but it can gradually affect how you feel and function.
Many people with obesity experience:
- Breathlessness
- Tiredness
- Low energy
- Joint pain or
- Sleep problems like snoring and sleep apnoea.
Emotionally, obesity can take a toll too, often leading to low self-esteem, anxiety, or depression. Over time, the physical effects of obesity can lead to much more serious health complications.
Diagnosis and measuring obesity
Common methods of assessment include:
Body Mass Index (BMI)
- 18.5–24.9: Healthy weight
- 25–29.9: Overweight
- 30–34.9: Obese (Class I)
- 35–39.9: Obese (Class II)
- 40+: Obese (Class III or severe obesity)
Waist circumference
Risk is increased in men with >94 cm (37 inches) and in women with >80 cm (31.5 inches).
Body fat
Body fat percentage is assessed with body composition tools.
Blood tests
Blood tests to assess metabolic health, insulin resistance or prediabetes.
Link between obesity and type 2 diabetes
Obesity is the most significant modifiable risk factor for type 2 diabetes.
In fact, around 80–85% of people with type 2 diabetes are overweight or obese.
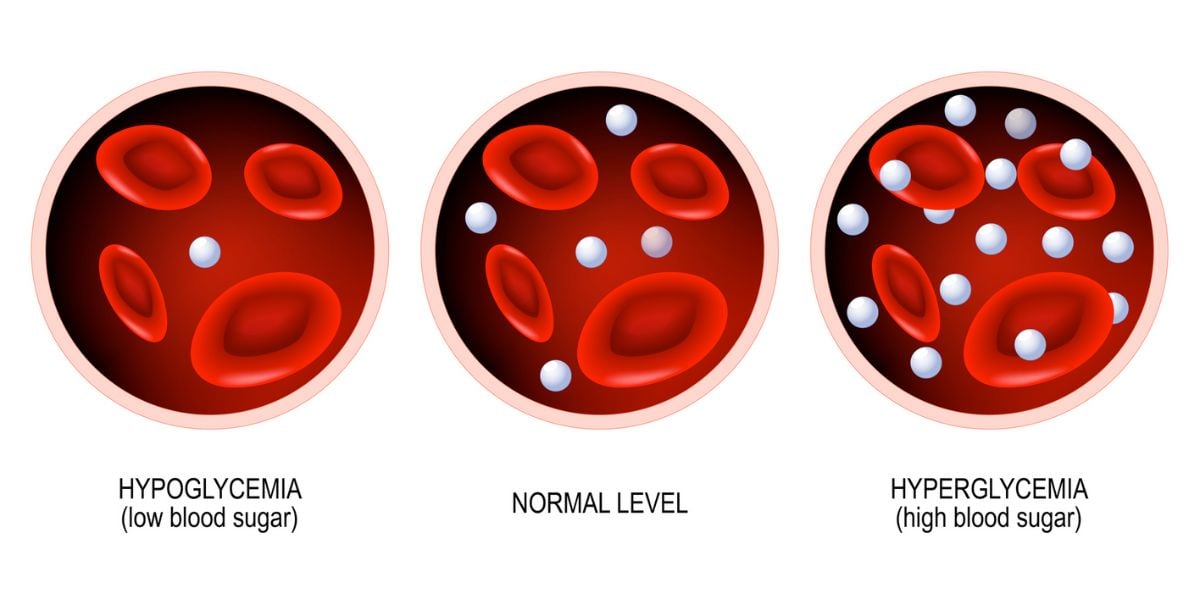
When there’s too much fat — particularly around the belly — the body’s cells can become resistant to insulin, the hormone that helps regulate blood sugar.
This condition, known as insulin resistance, means glucose builds up in the bloodstream, eventually leading to type 2 diabetes if not managed.
Research shows that people with obesity are up to 80 times more likely to develop type 2 diabetes than people with a BMI under 22.
Central obesity where one carries excess fat around the waist is particularly high risk.
Even before type 2 diabetes develops, many people pass through a stage called prediabetes, where blood sugar levels are raised but not high enough to be classed as diabetes. Prediabetes is often reversible, especially with early intervention and weight loss.
Other health risks associated with obesity
Obesity increases the risk of a wide range of serious conditions. These include:
- Type 2 diabetes with a 3–7x higher risk
- Cardiovascular disease (CVD) due to increased risk of stroke, hypertension, heart attack
- Breast, bowel, pancreatic, liver, and endometrial cancer
- Osteoarthritis due to increased wear and tear on joints
- Infertility, especially in women (linked to PCOS)
- Sleep apnoea, due to fat deposits around the neck
- Mental health disorders such as depression, anxiety, and low self-esteem
Can obesity be treated?
Yes — obesity is treatable and even modest weight loss can have a major impact on your health.
A 5% reduction in body weight can significantly improve insulin sensitivity, reduce blood pressure and lower cholesterol levels.
This in turn reduces your risk of developing type 2 diabetes by more than 50%, according to NHS data.
Lifestyle changes
Treatment starts with lifestyle changes.
A healthy, balanced diet that is lower in processed foods and refined sugars, combined with regular physical activity, forms the foundation.
Behavioural strategies — like tracking your meals, setting goals and managing emotional eating — can also help.
Structured digital tools like the Gro Health app can support these lifestyle changes by providing personalised support, education and motivation.
- Mediterranean Diet and 7 Day Meal Plan
- Low Carb Diet: Beginner’s Guide
- Intermittent Fasting: Guide to Fasting and How it Works
Weight loss medication
In some cases, medications such as GLP-1 receptor agonists may be prescribed including:
These medications help regulate appetite and have shown significant weight loss results in clinical trials. For those with severe obesity or related health complications, bariatric surgery may be considered.
Obesity in children and young people
Obesity is no longer an adult-only issue.
Worryingly, it’s becoming increasingly common in younger age groups.
Nearly a third of children aged 2 to 15 are now classed as overweight or obese and children from more deprived communities are disproportionately affected.
Obesity during childhood is likely to continue into adulthood and increases the risk of developing health problems earlier in life, including type 2 diabetes, heart disease and mental health issues.
Prevention through healthy eating, physical activity and education is critical — not only for the child but for the entire family.
Tackling obesity
Obesity prevention requires action on multiple fronts.
This includes education around healthy eating and physical activity, creating supportive environments in schools and communities and ensuring that people can access affordable, healthy food.
Local councils and healthcare providers are increasingly offering weight management services tailored to different cultural backgrounds and life stages.
The government and NHS also recommend routine screening for obesity and associated conditions.
Many GPs and local health services can refer people to weight management programs, including structured education, dietitian support and digital tools.
What is the cost of obesity?
Obesity costs the NHS an estimated £6.5 billion each year — and this figure is expected to rise to over £9.7 billion per year by 2050 if trends continue.
Much of this cost is related to treating obesity-related diseases, including:
- Type 2 diabetes
- Kidney disease
- Amputations
- Heart disease
- Cancers linked to obesity
Preventing obesity, or treating it early, can dramatically reduce the burden on the NHS and improve quality of life for millions.
Research highlights and new findings
Recent studies have shown that habits like late-night snacking, poor sleep during adolescence and maternal obesity during pregnancy can increase the risk of obesity in children and teens.
Sleep, in particular, plays a vital role in regulating hunger hormones and metabolism.
Studies also suggest that reducing screen time — even by just a few hours a week — can have a measurable effect on children’s waistlines.
- Preadolescent obesity risk in offspring reduced by breastfeeding
- Whole milk associated with reduced risk of obesity
- Countries with highest obesity levels revealed
Obesity is complex but it’s not inevitable.
The more we understand the contributing factors, the better equipped we are to support individuals and families on their journey toward healthier living.