Genetic predisposition
Researchers have uncovered a number of genetic regions that are linked closely with type 1 diabetes. Each of these is denoted with a name such as IDDM1. At least 18 different regions have been discovered and some of the genetic areas include an increased susceptibility for other autoimmune diseases such as rheumatoid arthritis and coeliac disease Whilst genetics offers clues as to why some people are more susceptible to type 1 diabetes, it doesn’t explain why some people with these genes develop type 1 diabetes and why others with these genes don’t. For example, having an identical twin with type 1 diabetes gives you a statistically higher risk but it doesn’t necessarily mean you will develop the condition. Genetics does not explain either why people will develop type 1 diabetes at different ages. Type 1 diabetes is most commonly diagnosed in 10 to 14 year olds but can be diagnosed at any age.
- Read more on diabetes and genetics
Type 1 diabetes triggers
Researchers have hypothesised that whilst some people are have a genetic predisposition to type 1 diabetes, there is likely to be an environmental factor that triggers the initial development of type 1 diabetes. Some of the possible triggers that have been suggested include:
Viral infection
Associations have been found between type 1 diabetes and a number of different viruses. Of these, enteroviruses have attracted the most interest from researchers. Studies have shown that enterovirus antibodies have been recorded at higher levels in pregnant mothers of children that gone on to develop type 1 diabetes. Higher frequencies of enterovirus infections have also been detected in children which develop type 1 diabetes when compared with siblings that have not developed the condition.
Vaccinations
Another theory put forward is that childhood vaccinations could increase the chances of developing type 1 diabetes. One researcher, Dr J B Classen has investigated incidences of type 1 diabetes in the human population as well as in animals. Dr Classen’s research indicates there could be a link between type 1 diabetes and childhood vaccinations such as smallpox, tuberculosis and Hib vaccines. The research has yet to be accepted as conclusive enough to change vaccination schedules.
Vitamin D
A link between vitamin D and type 1 diabetes has been drawn. Researchers have noted that countries with the highest incidences of type 1 diabetes tend to be located further from the equator. Countries such as the UK, Canada, Australia and the countries of Scandinavia all have notably high rates of type 1 diabetes. Studies have also shown that people with lower levels of vitamin D had a higher incidence rate of developing type 1 diabetes. A number of studies, including the EURODIAB Substudy 2, have shown that supplementation of vitamin D appears to lower the risk of developing type 1 diabetes.
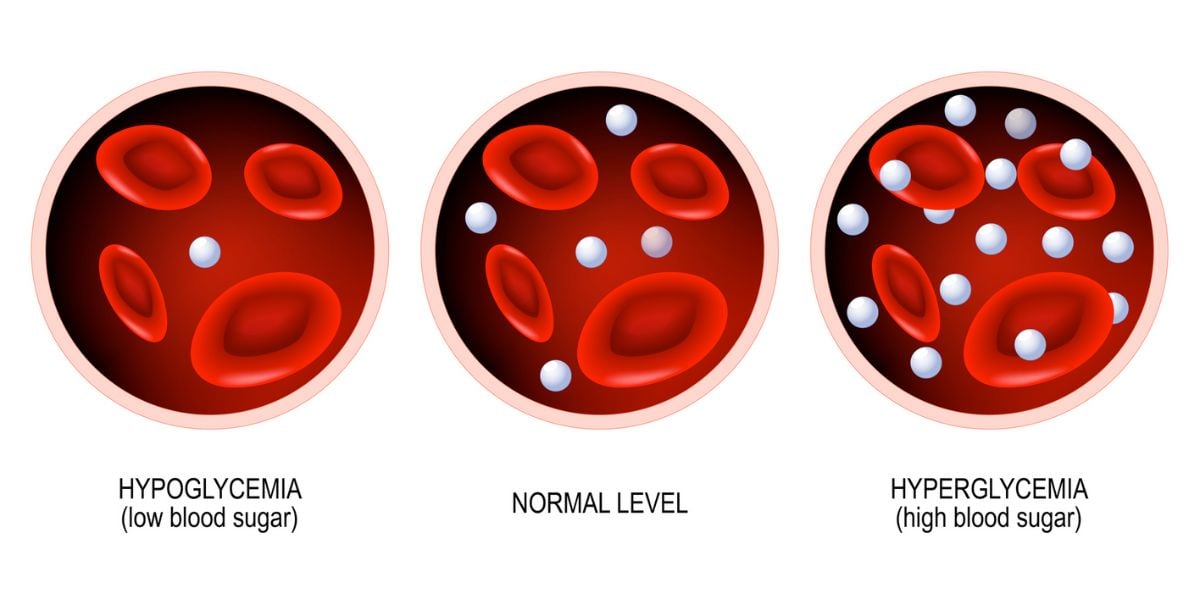
Increased insulin demand
Increased demand on insulin has also been put forward as a contributing factor. A study, carried out by the University of Colorado and published in 2008, showed that a diet with high glycaemic index foods could speed up the progression to type 1 diabetes in children with signs of islet autoimmunity. The growth phase that children go through in teenage years increases the amount of insulin released and could lead to extra stress on beta cells, raising the risk of the immune system attacking the insulin producing cells.