If you are diabetic and treat your diabetes with insulin, hypoglycemia whilst driving may be one of your biggest concerns.
Having a hypo whilst driving is both frightening and dangerous so it’s important that hypoglycemia is avoided.
If you have type 2 diabetes and treat your diabetes with certain tablets, there is also the chance that you may experience a hypo whilst driving.
Which diabetes medications can cause hypos?
The following diabetes medications can cause hypoglycemia.
The DVLA must be informed if you are a driver and take the following medications:
- Insulin
- Sulfonylureas
- Prandial glucose regulators
How to avoid becoming hypo whilst driving
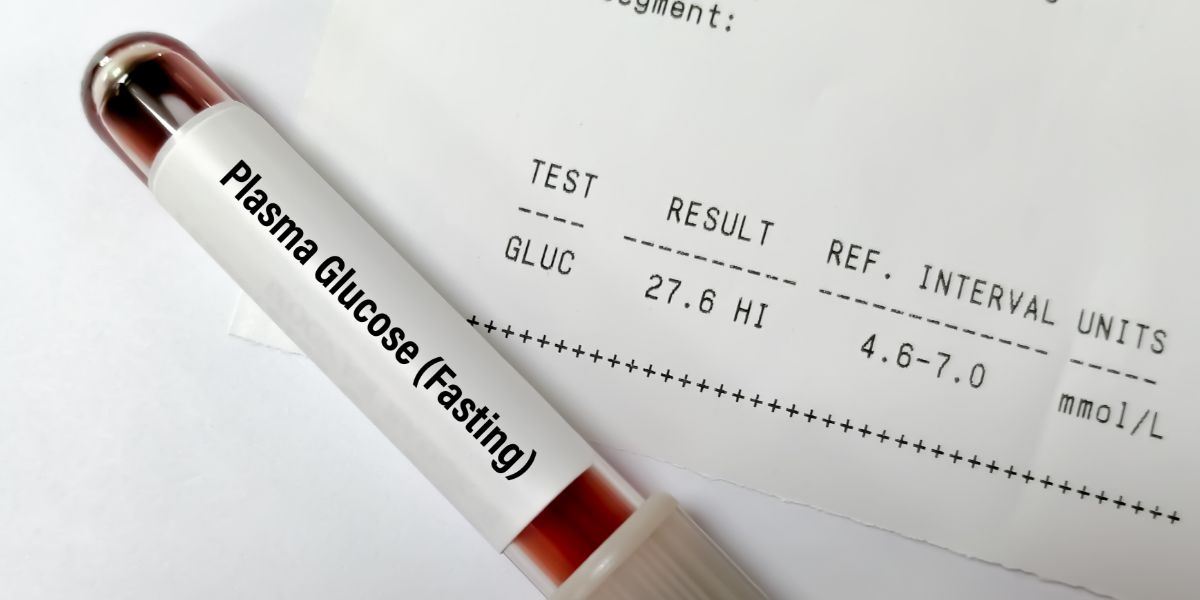
- Always test your blood sugar before driving
- Take regular breaks to test your blood sugar
- Do not drive with blood sugar levels under 5 mmol/L
- If you have a bad hypo, treat the hypo and do not drive until 45 minutes after your blood sugar has risen above 5 mmol/L
- Avoid driving when tired or on medications that may cause drowsiness
- Have glucose tablets or sweets to hand
- Never drink and drive
Even for short journeys hypoglycemia can be dangerous, so test before each journey. Shopping can lower blood glucose so test before the journey back as well as before the journey there.
It is recommended to take a break at least every 2 hours to test your blood sugar and to have a carbohydrate based snack if needed.
If you are tired or taking medication that may induce drowsiness, feeling lethargic will not only make you less alert on the road but could affect your ability to recognise low blood sugar as well.
Learn more hypo symptoms linked to driving and how to prevent lows when driving. Join the (free) Hypo Awareness Program »
Treating a hypo during a journey
If you notice signs that your blood sugar is low or you are otherwise concerned you may be low during a journey, find a safe place to stop and park.
Remove the ignition key and move into the passenger seat. This is to avoid any suggestion that you may be “under the influence” whilst in charge of a car.
If you are low, treat the hypoglycemia with fast acting glucose and sufficient slower acting carbohydrate to ensure your blood glucose levels are at a safe level for the rest of the journey.
Do not drive on until at least 45 minutes since your blood sugar has risen above 5 mmol/L and you feel fully alert. Following hypoglycemia judgements may be impaired for up to 45 minutes so you need to give your body plenty of time to recover. [84]
Hypoglycemia symptoms whilst driving
As hypoglycemia whilst driving is a dangerous situation, it’s essential to be aware of your hypo symptoms. If you notice any change in how you’re feeling or your ability to concentrate, make hypoglycemia your first consideration.
Common symptoms whilst driving could include:
- Staying in lane may take more concentration
- Finding it more difficult to focus your eyes
- Changes in body temperature – having a warm flush or suddenly feeling cold
- Starting to feel tired and/or yawning
- Feeling a tingling sensation, particularly in your fingers, lips or tongue
- A rise in your heart beat
- Feeling hungry
- Difficulty making decisions
- Stronger emotions than usual, such as angry, frustrated, worried, confused
If you notice one of these symptoms, take a break and test your blood sugar. Try to remember to remove the key from the ignition and test in the passenger seat as advised above.
Hypo awareness and driving
If you suffer from hypo unawareness, that is you have difficulty recognising hypo warning symptoms, the DVLA states that you should not drive.
If hypo awareness recovers, you may resume driving but the recovery of hypoglycemia awareness must be confirmed by a consultant or GP
Can hypoglycemia affect my licence?
You must inform the DVLA if you have had any episodes of hypoglycemia requiring assistance (termed as disabling hypoglycemia) within the previous year.
You should also inform the DVLA if your awareness of hypoglycemia has become impaired.
What if I have an accident whilst hypo?
If you have an accident whilst you are hypoglycemic, you should get legal advice and the support of your diabetes care team