Researchers from Moffitt Cancer Centre hope to improve the survival rates of patients with pancreatic cancer using blood marker diagnostic tools. The markers, they argue, can be used to identify patients with intraductal papillary mucinous neoplasms (IPMNs), a kind of premalignant pancreatic lesion which can indicate the impending onset of pancreatic cancer.
Pancreatic cancer is strongly linked with diabetes. Having diabetes increases the risk of pancreatic cancer, and having pancreatic cancer increases the risk of diabetes. Pancreatic cancer accounts for around three per cent of all cancer cases, and it has one of the lowest survival rates.
This study hopes that, with the right diagnostic tools, it will be possible to significantly increase the survival rate of pancreatic cancer patients.
“One promising strategy to reduce the number of people affected by pancreatic cancer is to identify and treat premalignant pancreatic lesions,” said first author Jennifer Permuth-Wey, assistant member in the Departments of Cancer Epidemiology and Gastrointestinal Oncology at Moffitt.
“IPMNs are established precursor lesions to pancreatic cancer that account for approximately half of all asymptomatic pancreatic cysts incidentally detected by computerised tomography (CT) scans or magnetic resonance imaging (MRI).”
The presents of IPMNs does not necessarily suggest that someone will develop pancreatic cancer; some IPMNs are less dangerous than others. IPMNs are categorised as being either low-risk or high-risk, but these categorisations tend to be imprecise. The only reliable way to judge the severity of IPMNs is by removing them, but this is associated with several other complications – diabetes chief among them. However, neglecting to remove them can lead to the development of avoidable pancreatic cancer.
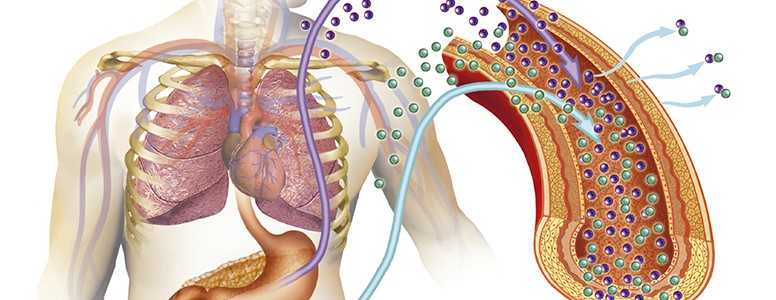
The researchers aim to address this difficulty. They want to develop efficient blood tests to accurately distinguish between low-risk and high-risk IPMNs, so that medical professionals can say with certainty which lesions should be removed and which shouldn’t. To do this, they examined microRNAs (miRNAs), molecules that regulate the genes that are responsible for the development of cancer.
Senior author Mokenge Malafa, department chair and program leader for Moffitt’s Gastrointestinal Oncology Program, said: “Using new digital technology, we compared the expression patterns of miRNAs in the blood and discovered a set of 40 miRNAs that differentiated between IPMN patients and healthy volunteers. We also identified five miRNAs that could distinguish between high-risk IPMNs and low-risk IPMNs.”
In other words, certain miRNAs appear to able to tell the difference between high-risk IPMNs and low-risk IPMNs, meaning that, with more work, they could be used to detect possible cases of pancreatic cancer before they develop. That said, the research is currently at a preliminary stage.
“We are excited about our preliminary findings, but much more research is needed before such a blood test could be made available in the clinical setting,” said Malafa.
“The hope is that in the not-so-distant future a miRNA-based blood test can be used in conjunction with imaging features and other factors to aid the medical team in accurately predicting disease severity of IPMNS and other pancreatic cysts at the time of diagnosis or follow-up so that more informed personalised medical management decisions can be made.
“Early detection and screening are the most effective ways for ‘at-risk’ individuals to minimise the potential for developing pancreatic cancer.”
The finding were published in Cancer Prevention Research.
What's new on the forum? ⭐️
Get our free newsletters
Stay up to date with the latest news, research and breakthroughs.