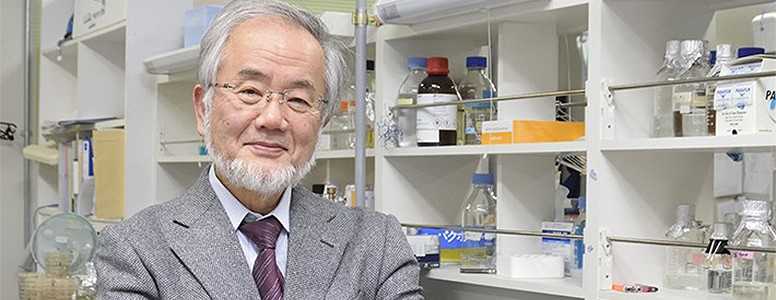
The Japanese cell biologist Yoshinori Ohsumi has won the Nobel Prize in Physiology or Medicine for his work on the role of cellular recycling in metabolic diseases that involve altered mitochondrial function, including metabolic syndromen, diabetes, and obesity.
The new Nobel laureate from the Tokyo Institute of Technology in Japa, was given the award for pioneering research on an essential intra-cellular degradation system known as autophagy, that keep cells healthy.
Honorary Professor Yoshinori Ohsumi’s discoveries revolve around how the autophagy process, whereby the body’s cells break down and recycle their own components, can become deficient and lead to many diseases.
The process of autophagy can influence other cellular processes like cell death and proliferatio, and if dysfunctional, can cause neurodegenerations, cancer, and infections.
It has also been suggested that autophagy may impact glycogen (glucose stored in the muscles) and lipid metabolism, as well as the regulation of underlying inflammatory responses that a lot of metabolic disorders, such as diabetes, insulin resistance and obesity, have in common.
More recent studies looking at the reversal of these diseases and even the progression of ageing have shown how autophagy can be turned on in the cells as part of a molecular reset switch to repair damages or ensure survival during a fasting state.
These findings have had huge implications for our understanding of which diet and lifestyle habits, like intermittent fasting, are capacitating such cell renewal processes.
One study found, for example, that an autophagy-dependent process called glycophagy in the heart tissue during fasting could offer protection against diabetic cardiomyopathy.
In his latest works, published in Developmental Cell, Ohsumi has clarified the starvation-induced mechanisms and selective pathways of autophagy as well as all the specific genes involved in this process.
The Japanese researcher started researching and documenting autophagy in 1977 in yeast, which is considered a good model for human molecular biology as it shares a network of similar autophagy-related proteins or ATGs.
It took a long time for the autophagy field to become popular, but it sparked a lot of interest once Ohsumi identified that these ATG genes found in plant cells are also present in mammalian cells.
This has led to the expansion of autophagy research from yeast to mouse and human biology with evidence that autophagy is an interesting component of so many physiological events in the body.
The researcher has found that autophagy is, for instance, important for the elimination of intracellular harmful proteins damaging mitochondrias, the powerhouses of the cell that shape metabolism and healthy ageing.
In pancreatic beta-cells, specifically, studies have shown that the deletion of Atg7 (among the ATGs needed for the authophagic process) resulted in mice that were hyperglycemic, glucose intolerant and had a decline in insulin production. The absence of Atg7 was also associated with a decline in kidney function.
Overall Ohsumi’s findings have provided new insights for researchers studying mitochondrial dysfunction and how genetic interferences of ATGs in the liver, fat tissue, and elsewhere in the body may be implicated in a variety of diseases like type 2 diabetes and obesity.
Image source: ohsumilab.aro.iri.titech.ac.jp
What's new on the forum? ⭐️
Get our free newsletters
Stay up to date with the latest news, research and breakthroughs.