A chemist from Boston University College of Arts and Sciences has recently won a $1.4 million National Institutes of Health (NIH) grant for repurposing post-transplant immunosuppressants as a shield against autoimmune attacks to the pancreas in type 1 diabetes.
Arturo Vegas first earned the equivalent of five years of research funding from the NIH in September of last year, through their New Innovator Award. At the time, Vegas already worked towards developing immunosuppressant therapies targeted at pancreatic islets.
The latest grant he received, as part of the Type 1 Diabetes Pathfinder NIH Award, complements his ongoing efforts to find exactly how repurposed immunosuppressive drugs could work to effectively protect beta cells.
Vegas always believed that such a strategy could yield better results than conventional type 1 diabetes therapies, as it is an early intervention in the disease development process.
His idea also opens up a whole new avenue of investigatio, as much of type 1 diabetes research that is currently being funded revolves around compensating for the loss of beta cells with therapies which appear hard to replicate or scale up to be useful for people in a near future.
Vegas’s goal is precisely to render superfluous late stage therapies like the implantation of insulin-producing cells, by putting our best efforts to preserve a patient’s own beta cells against rogue immune cells from the start.
And for Vegas, this could be achieved through the action of immunosuppressants acting in a way that doesn’t target the whole body but just sites of the pancreatic islets that are under autoimmune attacks.
For this purpose, Vegas hopes to create a sort of reconnaissance system for immunosuppressants, whereby small molecules attached to the drugs would bind to receptors present on the surface of insulin-producing cells.
The active compound of the drugs would therefore only go to that space and remain there to guard against bad immune cells trying to do harm.
According to Vegas, this could prove to be a very effective prevention strategy if it is used in the early stages of type 1 diabetes.
Another area of research Vegas is looking into has to do with the design of a molecule able to localise pancreas-attacker cells, thanks to a special protein they carry, and destroy them before they do any damage.
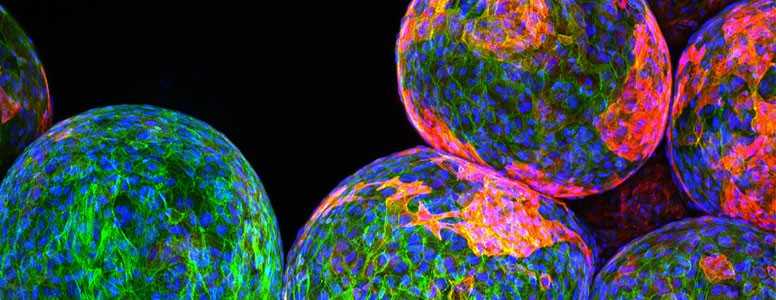
Photo: Boston University
What's new on the forum? ⭐️
Get our free newsletters
Stay up to date with the latest news, research and breakthroughs.