New research published in the leading British Journal of General Practice, shows that the Low Carb Program supports sustainable weight loss, improvements in glycemic control and medication reduction in people with prediabetes or type 2 diabetes.
Researchers from University of Warwick worked with four GP practices in the West Midlands and followed eligible patients with prediabetes or type 2 diabetes who were offered access, or signposted, to the Low Carb Program at a routine consultation.
Rates of offering and accepting signposting were recorded, with program registration, program completion and health outcomes.
Of 351 patients offered signposting, 45.6% of patients accepted a referral from their GP or healthcare professional. GPs reported signposting took between 1-4 minutes.
Remarkably, almost twice as many participants from Black and Asian ethnic groups accepted signposting when compared to their white counterparts.
- Low Carb Program with remote clinical appointments shown to be as effective as face-to-face obesity weight management services
- Low Carb Program shown to be effective in improving glycemic control and enabling weight loss
Just over 1 in 4 participants who accepted signposting completed the Low Carb Program.
Patients completing the program reported greater weight loss (7.2kg) and HbA1c improvements (-9.1mmol/mol) compared to those who did not, and were more likely to reduce the number of general practice-prescribed diabetes medications. Over 6 in 10 participants (62%) reduced medications at follow-up.
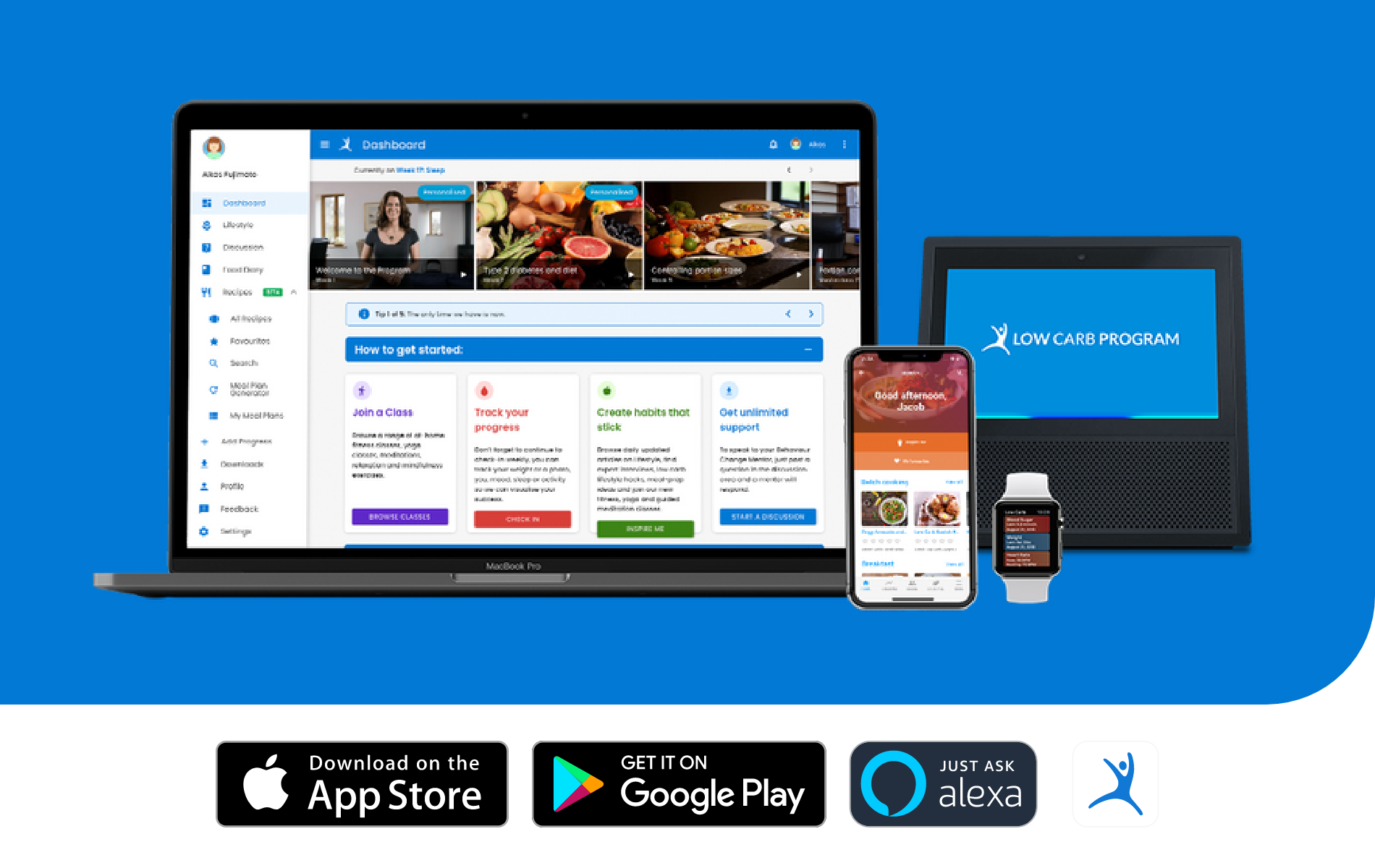
The Low Carb Program is an nutritionally-focused behaviour change intervention that provides education, resources and support to start and sustain a lower-carbohydrate diet. Low Carb Program is the highest Orcha-rated diabetes app (94%, 2021).
The app provides structured education, and long-term behaviour change support to support patients to achieve self-selected health goals by reducing the amount of carbohydrates to 130grams a day.
App features include a goal-focused tailored education programme, peer coaching, recipe library (including cook-a-longs), live and on-demand activity classes and health tracking.
Charlotte Summers, Chief Operations Officer at DDM said: “We’ve empowered over a million people to make better decisions, and we are delighted to demonstrate how Low Carb Program can support patients with prediabetes and type 2 diabetes to achieve positive health improvements.”
The app is used by patients with obesity, pre-diabetes, type 2 diabetes, non-alcoholic fatty liver disease and polycystic ovarian syndrome. The program is evidenced in 5 peer-reviewed studies.
The app supports over 60 cultural food preferences and is available in 9 languages: English, Hindi, Punjabi, Arabic, Gujarati, Bengali, Tamil, German and French to democratise access to health and care.
Professor Jeremy Dale commented: “This research demonstrates the feasibility of referring patients with prediabetes or type 2 diabetes from primary care consultations to digital services that support weight loss like the Low Carb Program. In particular, the engagement with BAME communities should be further explored.”
Dr Peter Foley, Clinical Safety Officer at DDM commented: “As an NHS GP, I am acutely aware of the current difficulties which patients and clinicians are faced with. Very often, these difficulties can be dramatically improved through lifestyle optimisation. The Low Carb Program has been shown to empower patients with pre-diabetes and type 2 diabetes to make sustained and improved lifestyle habits. The resulting improvements in weight and blood sugar control not only improve users’ health and wellbeing, but also reduce the economic prescribing burden for local health authorities.
“We are particularly encouraged by the engagement of users from the BAME community, as we believe that everyone deserves equal access to our award-winning tool, no matter their background, culture or ethnicity.”
The research team comprised Dr Emma Scott, Mishkat Shehata, Charlotte Summers, Arjun Panesar and Professor Jeremy Dale.